Wanda knows she’s being poisoned.
The nurses come to her room and tell her to breathe from a tube, and Wanda can see glass particles entering her lungs.
So she refuses to inhale. Sometimes her doctor, whom Wanda trusts, convinces her to relent and breathe the stuff in. Other times she stays strong.
Roughly six times in the last six months, Wanda has stayed strong. Each time, her lungs began to fill with fluid—an effect of the congestive heart failure she suffers from. Each time, she has had to be restrained, intubated, and cared for at Legacy Emanuel Medical Center, causing her immense psychiatric trauma. The last time this happened, Wanda nearly died.
On a late April morning, as an array of mental health workers, attorneys, and court officials meet to talk about her in a tidy room at Portland’s brand-new Unity Center for Behavioral Health, Wanda has refused to breathe the glass poison for days. Another trip to Emanuel may be necessary, but that’s not the reason for the day’s hearing.
Instead, the group has gathered to determine whether Wanda, who’s in her 60s, should remain in state custody.
For much of the last six months, she has been one of a rising percentage of patients in Multnomah County committed against their will to the care of the Oregon Health Authority (OHA), which believes the paranoid schizophrenia Wanda suffers from puts her at dire risk.
Today, her first stay is nearly up, and the state is deciding whether Wanda should be recommitted for another 180 days—the maximum length for a single commitment.
“I don’t believe she would voluntarily take her medicine,” says Wanda’s psychiatrist, Dr. James Russell, who explains the woman’s notions that her medication—delivered as a mist—is killing her. Two mental health experts briefly interview Wanda to get a sense of her grasp on reality. A county prosecutor says Wanda needs to stay in the state’s hands; a public defender half-heartedly argues she should be freed.
For Portland, the decision a county judge will make at the end of the hearing will help decide whether the city’s overtaxed mental health system works as hoped.
More and more, county officials say, the system set up to cater to the city’s most pressing mental health crises is devoting much of its time to serving people like Wanda—patients with severe illness who aren’t currently able to care for themselves or could pose a danger to others.
The reasons are varied, and not entirely clear, but the difficulties are apparent. Just as the innovative Unity Center is working to improve the way Portland addresses the crises of a rapidly expanding population, the influx of serious cases ties up precious resources.
“They need long-term care,” says Dr. Y. Pritham Raj, a Unity board member and chair of the Department of Behavioral Health at Adventist Health. “That’s not what Unity was designed to be.”

Bill Osborne looks at the whiteboard hanging in his office and can’t help but think something’s changed.
As the supervisor of Multnomah County’s Commitment Services program, Osborne oversees a staff responsible for deciding whether to pursue civil commitments for thousands of patients they encounter each year.
When they do ask for a commitment hearing, it goes on Osborne’s board. And lately, the board has been routinely full.
“Tomorrow I have three,” Osborne said in a conversation last month, noting that his investigators are seeing more severe cases lately. “I wish I could tell you why that was happening,”
The data Osborne points to is limited but, to his thinking, worrisome. It shows that in January and February of this year, county investigators have been seeking to commit patients at roughly twice the typical rate—an increase he says isn’t tied to any policy change.
Civil commitment to state custody is designed to be a last resort, necessary when a person with mental illness is a danger to themselves or others, or incapable of providing for their own basic needs. And because commitment involves stripping a person of their civil liberties, the process is complicated.
“The bar in Oregon to get someone civilly committed is very high,” Osborne says. “We are seeing people who are more acutely ill, and who are meeting that bar.”
Often, the machinery of civil commitment kicks into gear when local cops or qualified social service workers get a call about someone in crisis. If the situation is severe enough, those officials will bring that person to a local hospital, where a doctor can make the decision to hold them for up to five business days by issuing a “notice of mental illness.” It’s at that point that Osborne’s investigators come on the case.
In recent years, the staff has investigated between 3,500 and 4,400 people. And in each of the past five years, the county has recommended between 6 and 7.5 percent of those people be civilly committed (the overwhelming majority ultimately are), according to county records.
But this year, that ratio has shot up. According to county data, more than 15 percent of the people investigated in January and February faced a commitment hearing.
“Seeing that kind of spike in civil commitments is concerning,” Osborne says. “It’s something we’re not used to.”
He’s the first to admit the numbers could be a blip—the mental health system ebbs and flows, after all—but there’s something Osborne also feels compelled to point out.
“These are not the same people we’ve seen again and again,” he says. “We’re seeing a lot of people from out of town.”
He’s got a theory on why that might be.

Before we look at Osborne’s out-of-towner observation, though, consider why an increase in commitments matters.
Until this year, when people in Portland were in the midst of a serious mental health crisis, they had little choice but to wind up in the emergency department at one local hospital or another—the same ERs that house people with other pressing emergencies.
“It’s not a peaceful, calming, reassuring environment,” says Dr. George Keepers, a board member for the Unity Center and chair of the psychiatry department at Oregon Health & Science University (OHSU). “It is not a good place for psychiatric patients to stay.”
Prior to late January, those patients might be stabilized and sent home. Or they might be admitted to wards designed specifically to help people grappling with acute psychiatric problems (a persistent criticism of mental health advocates is that our system doesn’t have enough resources in between those two options). Often hospital beds were full, meaning patients would need to wait in the chaos of the ER for one to open.
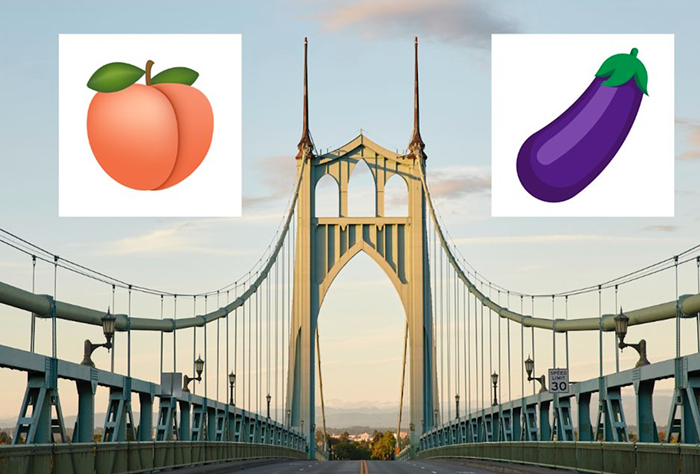
The Unity Center—which opened on January 31, just across I-5 from the Moda Center—was envisioned as an upgrade. First announced in early 2015, the center was developed as a partnership between four major health care providers: OHSU, Legacy Health, Adventist Health, and Kaiser Permanente.
The hospital systems pooled funding and transferred their local psychiatric beds to Unity, culminating in 102 inpatient beds (80 for adults, 22 for children), which is actually a net loss of 10.
Even so, officials believed the facility could offer significantly better outcomes for one central reason: At Unity, patients enter an emergency ward purpose-built for people in mental health crisis.
“Now they have someone immediately talking about care, talking about medications,” says Amber Shoebridge, a spokesperson, who described the facility’s emergency wing as “roomy” and “light,” but declined to give the Mercury a tour. Prior to Unity, she says, the process was more “you stick me in a room and isolate me, and I don’t get help for however long. Anxiety goes up.”
And while this new model is winning over mental health providers who believe it’s a better option for patients, the center is still finding its feet.
Hospital officials envisioned that 75 percent of people who walked through the door would require emergency attention of 24 hours or less. The remaining patients would be stabilized in the center’s inpatient beds for no more than eight days, and then released with a treatment plan.
On average, that’s not happening—and one big reason is patients like Wanda. According to officials, 40 percent of the adult beds at Unity are currently taken up by civil commitments.

It’s not uncommon for committed patients to stay at the center for a month or more. And while they’re people absolutely in need of the type of care Unity provides, any increase can constrain the system’s limited resources.
“If you have a high percentage of beds occupied by patients who are staying 30 days or longer, that shifts the average length of stay fairly quickly,” says Keepers. “It slows down the throughput of the hospital.”
People who require inpatient care currently wait an average of nearly two days in recliners in the Unity Center’s emergency wing before receiving a bed.
And since patients with mental health issues are still showing up to emergency rooms around the city, they’re still sometimes being “boarded” at those hospitals until space opens up at Unity—that “stick me in a room and isolate me” scenario Shoebridge referred to. The Unity Center refused to release data to the Mercury showing how long people are waiting in hospitals before being transferred to the facility, stressing that the system is still in its infancy.
“There’s a chain reaction.You’ve got all these people committed, and you don’t have a place to put them.”—Dr. Y. Pritham Raj
To be clear, unmet demand for mental health beds is nothing new for Portland.
There have never been enough resources, or even the right kinds of resources, for handling all the people experiencing crisis at a given moment in the city. Add the fact that the population is growing rapidly—and that, according to federal data, roughly four percent of all adults in the US experience serious mental illness—and it makes sense that Portland is still seeing difficulties.
The question is how to solve them.
“There’s a chain reaction,” says Raj. “You’ve got all these people who are, say, committed, and you don’t have a place to put them.”

Christopher doesn’t know that he is 50 years old, or what time of year it is. He believes his family has been replaced by impostors, and that his estranged wife, who is still alive, died “weirdly, Walking Dead-style.”
At home, Christopher would sometimes hear assailants banging on his door and walls. He believes people who walk by his house are spying on him with ill intent. He insists he’s been blacklisted from getting any sort of job.
Until March, Christopher lived for more than a decade with his elderly mother and sister, in a home one police officer describes as resembling an episode of Hoarders: layers of grime on the counters, trash piled on the floor.
Then on March 31, Christopher took a crowbar to his mother’s locked bedroom door in search of batteries, and struck his sister repeatedly when she tried to intervene. The police showed up to the house weeks later—after the mother and sister had fled—and took Christopher to the hospital. At some point, he was transferred to Unity.
On April 25, he is brought, shoeless and unkempt, into the bright courtroom where civil commitment hearings at the center take place.
Christopher’s clinician tells the court the man is schizophrenic, and “not oriented to time or place or situation.” His sister, still visibly angry from the events of late March, testifies matter-of-factly that she and her mother have a restraining order against the man, and that he is no longer welcome to live with them.
Christopher, in a high-pitched, soft-spoken voice, explains there is nothing wrong with him. “I don’t have a problem,” he tells two mental health professionals asking him questions about his perceptions. “This happened for real.”
It doesn’t take long for a judge to commit him to OHA custody for up to 180 days. He is brought back upstairs. How long he’ll remain there is unclear.

You can’t talk to anyone about the problems in Portland’s mental health care system without hearing about the Oregon State Hospital.
Currently comprised of two main facilities—in Salem and Junction City—and built to accept roughly 800 patients, the OSH is where the state cares for some of those who’ve been civilly committed, but also for people who might be in prison if they didn’t have a mental illness or who need psychiatric care to understand criminal charges against them.
The hospital in Salem has seen plenty of notoriety in the past century—culminating in an investigation by the US Department of Justice that began in 2006 and continues to influence]. Still, since the decrepit original facility was torn down and a new one opened in 2011, much of the scandal has subsided.
And depending on whom you talk to, the OSH is either helping spur delays in Portland’s mental health system or is a potential answer for them.
Which brings us back to Osborne’s observation that his staffers are seeing more very sick people trickling in from out of town. “It feels to me these are not the same people we’ve seen again and again,” he says.
It’s a mere anecdote, of course, but Osborne doesn’t shy away from pointing to a potential factor: He believes the state hospital, keen on proving itself to the DOJ, is releasing people too early.
“We’re seeing people who are coming out of the state hospital who quickly decompensate and end up back in our system,” he says. “They’re discharging some really poor discharges.”
The sentiment is backed up by Raj, who says that Adventist experienced similar issues before transferring its 43 psychiatric beds to the Unity Center.
“Sick, sick patients were coming right out of long-term care,” he says. “The hope was if you stayed at the state hospital for three months, you’d be better. Sometimes you’d be coming out no better.”
Osborne and others the Mercury spoke with point to a state plan developed in partnership with the DOJ, called the Oregon Performance Plan, which sets aggressive targets for when the hospital releases patients.

By late June, for instance, the OSH is pledging to discharge 75 percent of people it deems “ready to transition” within 30 days. By 2019, 90 percent of those patients will be released within 20 days.
These benchmarks are part of a more comprehensive plan, and are designed to ensure people aren’t being kept in state custody longer than necessary. But for Osborne, they raise questions.
“It concerns me when you have an organization like that saying, ‘We have to discharge an amount of people in a certain period of time,’” he says. “Why? Is there housing for them?”
Mike Morris, the OHA’s behavioral health administrator, suggests that concern is overblown.
“You need to look at the Oregon Performance Plan in its entirety,” he says. “Yes, there’s a push to get people out of state hospitals, but there are also things to make sure people are prepared to go out into the community.”
Those include housing support, crisis services, and more, Morris says.
There are also those who say the hospital should be doing more to admit Portland patients, thereby freeing up local resources. It often takes weeks from the time a person is referred to the hospital until they are admitted, Osborne says.
Part of that is by design. Morris says the hospital doesn’t presume it will take in every patient committed to state custody, and wants to ensure everything possible is being done locally before admitting someone.
But a lot of it also comes down to resources. More and more, state numbers show, the hospital system is tied up with so-called “aid and assist” cases, in which clinicians work with accused criminals.
“That has impacted our ability to take civil commitments over the last year, year and a half,” says Morris. At any given time, the hospital has a list of a dozen civilly committed patients or more waiting to land a spot.
Keepers, the OHSU psychiatry chair, says the problem could be partly helped if the state fully staffed the hospital system, which is frequently criticized for its high costs.
“If it were to be fully opened, that would take quite a bit of pressure off the system,” he says, referring to the hospital facility in Junction City.
Instead, the state appears ready to go the opposite direction. In her efforts to close a $1.6 billion budget hole, Gov. Kate Brown has proposed closing the 174-bed Junction City facility next year, just three years after it opened.

It’s still too early, of course, to tell if the Unity Center will deliver on the hopeful fanfare it opened to in January.
And some close watchers of the mental health system are skeptical the center will offer that much progress in a city—and state—that lacks so many resources for helping people who aren’t either in dire emergencies or relatively stable.
“Conceptually it’s a nice option to have,” says Chris Bouneff, executive director of the National Alliance on Mental Illness of Oregon. “At the same time, we can’t be patting ourselves on the back. We’ve done one thing.”
Still, if Portland is going to be successful at helping increasing numbers of people in trouble on its streets, the Unity Center has to be a central piece in seeing them get compassionate and knowledgeable care. As Bouneff points out, there’s not an emergency room like it in the state. Simply the fact Unity was built is a positive indication.
“Ten years ago in this state, we wouldn’t even be having this conversation,” he says. “We wouldn’t be developing anything.”
Now, we have developed something. It just has to work.
Back at Wanda’s recommitment hearing, the judge doesn’t take much time to reach a decision: The woman still suffers from a mental illness, is incapable of caring for herself, and will be committed for up to 180 days.
It will be up to her doctor to convince Wanda to breathe in her medication, and to stave off another emergency trip to save her life. But with the verdict comes another thing the Unity Center must consider.
Wanda’s just been accepted to the state hospital. Now that she’s been recommitted, she can leave tomorrow.